Overwhelmed Facilities Lead to Premature Discharges
Hospital beds for mental health patients are in such high demand across New Zealand that individuals are frequently turned away or discharged prematurely, according to recent figures released by Te Whatu Ora Health New Zealand. Data for the northern region shows nearly 100 percent bed occupancy over a three-month period, a situation reflective of the national trend, though specific nationwide figures were unavailable.
New Zealand has approximately 1,309 funded mental health and addiction hospital beds, with 905 designated for acute mental health needs. The demand for these beds has reached unprecedented levels, leading to significant strain on both patients and their families.
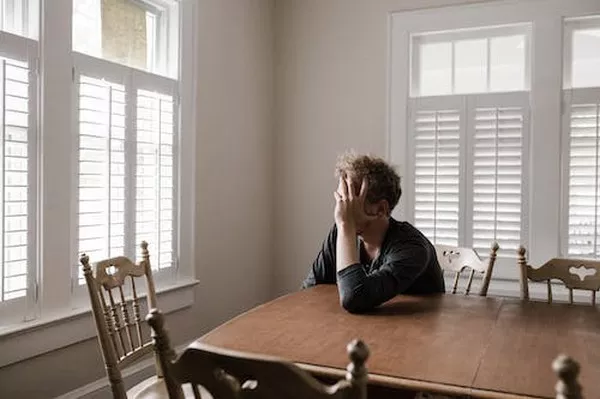
Families Bearing the Burden
John Moore, CEO of the Yellow Brick Road charity, highlighted the heavy burden placed on families due to the overwhelmed mental health services. “Families are being expected to pick up the slack, with patients discharged as soon as possible,” Moore said. He noted that sudden discharges have left families feeling ill-equipped to care for their loved ones, potentially damaging relationships and hindering recovery.
Yellow Brick Road advocates for increased investment in preventative and community-based services, in addition to the necessary funding for clinical and hospital services.
Staff Shortages Exacerbate the Crisis
Sarah Dalton, Executive Director of the Association of Salaried Medical Specialists, emphasized that staff retention issues are compounding the problem, creating unsafe conditions for both patients and staff. “There’s pressure on inpatient wards to discharge patients earlier to free up bed space for those acutely unwell,” Dalton explained. However, insufficient community support for early discharge patients exacerbates the issue.
High attrition rates, particularly among psychiatrists, have forced some facilities to reduce the number of available beds. This situation sometimes leaves acutely unwell patients in emergency departments for extended periods, further straining the healthcare system.
Government Response and Criticism
The government’s recent announcement of $24 million in funding for the mental health charity I Am Hope over four years has been met with disappointment by healthcare professionals, who argue that acute mental health facilities are in dire need of adequate staffing.
Despite efforts to build new or upgraded mental health facilities in various locations, including Palmerston North, Waikato, Christchurch, and Tauranga, there are concerns about whether these facilities will be sufficiently staffed to meet the growing demand.
Calls for Improved Data and Training
Dr. Hiran Thabrew, Chair of the Royal Australian and New Zealand College of Psychiatrists (RANZCP) national committee, pointed out the impact of overcrowding, particularly in child and youth services. “Most nights I’m on call, there are only one or two beds left,” he said, noting the difficulty in accommodating all who need care.
The RANZCP has called for increased funding for psychiatry training positions, expansion of services to match population growth, and a comprehensive stocktake of mental health services.
Te Whatu Ora’s Specialist Mental Health and Addiction Director, Karla Bergquist, stated that the organization is working to standardize nationwide reporting of occupancy data, with a new system expected by July. Current data collection methods vary across districts, complicating the aggregation of nationwide figures.
“Our staff are well equipped to manage high occupancy, which occurs regularly, and patient and staff safety is always our top priority,” Bergquist assured. She added that most districts have escalation processes in place for high occupancy situations, including the deployment of additional staff when necessary.
Conclusion
The high demand for mental health hospital beds in New Zealand underscores the urgent need for systemic improvements in both clinical care and community support. As Mental Health Awareness Month continues, it is vital to address these challenges to ensure that those in need receive timely and effective care.